US Quiz of the Month – April 2020
CASE REPORT
A 47-year old female patient with previous history of psoriatic arthritis, medicated with etanercept, was referred to our Gastroenterology Department due to episodic dysphagia to solids. The patient had already performed a computed tomography (CT) scan, which revealed a 3.5cm subcarinal nodular lesion, well circumscribed, hypodense with cystic areas, and without contrast enhancement.
For better characterization, a magnetic resonance imaging (MRI) was done and confirmed the subcarinal nodular lesion, with the same dimensions, well delimited, T1 isointense and T2 heterogeneous hyperintense, and with heterogeneous contrast enhancement (Fig. 1).
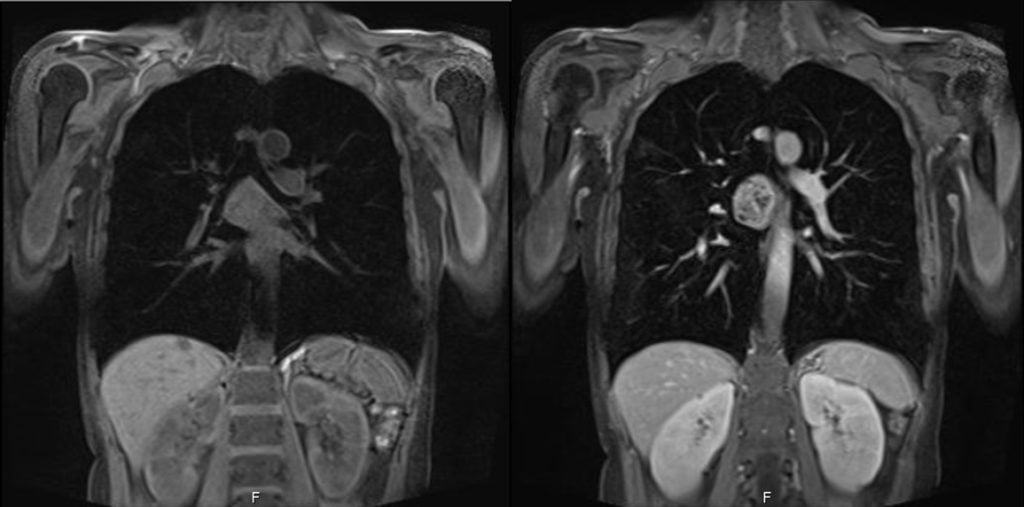
Figure 1. Thoracic MRI – T1 (left) and T2 (right) weighted images: subcarinal nodular lesion, with 3.5cm, well delimited, T1 isointense and T2 heterogeneous hyperintense, and with heterogeneous contrast enhancement.
Therefore, an endoscopic ultrasonography (EUS) was performed and documented, between 24 and 28 cm from the incisors, a hypoechoic and heterogeneous well delimited lesion in the esophageal wall, arising from the fourth layer (muscular propria), without invasion of the adjacent structures (Fig 2). A fine needle aspiration was made (3 passes with a 19G needle).
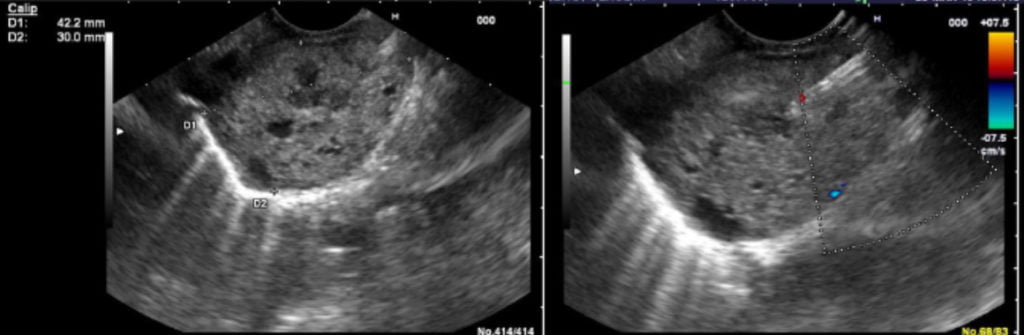
Figure 2. EUS (left) and EUS-FNA (right): hypoechoic and heterogeneous well delimited lesion in the esophageal wall, arising from the fourth layer (muscular propria), without invasion of the adjacent structures.
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
Cytological examination revealed aspects compatible with a benign nerve sheath tumor/schwannoma. Immunohistochemical staining was positive for S-100 and negative for desmin and α-smooth muscle actin.
Benign primary tumors of the esophagus are uncommon (2% of all esophageal tumors) [1]. The most common is leiomyoma [2]. Scwannoma of the esophagus is extremely rare with few cases reported in the literature [3]. The most common symptom of this condition is mild to moderate dysphagia, but dyspnea and chest pain can also occur depending on the tumor size. Actually many patients are asymptomatic and are incidentally found to have a benign esophageal tumor [2]. The diagnosis of a schwannoma is difficult with only imaging studies. Thus it is essential to obtain a tissue sample by endoscopic ultrasound-guided fine needle aspiration/biopsy (EUS-FNA/B). EUS-FNA/B is considered to be a safe, reliable, and accurate method for obtaining a tissue diagnosis in the evaluation of subepithelial lesions of the gastrointestinal tract, with minimal risks associated [4-5]. Surgical treatment for benign esophageal tumors arising from the submucosal layer is controversial. In general, surgical resection should be considered for large, symptomatic or increasing in size tumors [6]. Therefore an accurate preoperative diagnosis is crucial, leading to less invasive surgical treatment.
REFERENCES
- Kitada M, Matsuda Y, Hayashi S, et al. Esophageal schwannoma: a case report. World J Surg Oncol. 2013; 11:253.
- Moro K, Nagahashi M, Hirashima K, et al. Benign esophageal schwannoma: a brief overview and our experience with this rare tumor. Surg Case Rep. 2017; 3:97.
- Mizuguchi S, Inoue K, Imagawa A, et al. Benign esophageal schwannoma compressing the trachea in pregnancy. Ann Thorac Surg. 2008; 85(2):660-2.
- Okubo K, Yamao K, Nakamura T, et al. Endoscopic ultrasound-guided fine-needle aspiration biopsy for the diagnosis of gastrointestinal stromal tumors in the stomach. J Gastroenterol. 2004; 39(8):747-53.
- Klapman J, Chang KJ, Wiersema M, Murata Y, Vilmann P. Endoscopic ultrasound-guided fine-needle aspiration biopsy in esophageal cancer. Endoscopy. 2005; 37(4):381-5.
- Watanabe T, Miyazaki T, Saito H, et al. Resection of an esophageal schwannoma with thoracoscopic surgery: a case report. Surg Case Rep. 2016; 2:127.
AUTHORS
Manuel Rocha1, Sara Santos1, Diana Carvalho1, Gonçalo Ramos1.
- Gastroenterology Department, Centro Hospitalar Universitário de Lisboa Central, Lisbon, Portugal.


