US Quiz of the Month – fevereiro 2025
Case Report
We present a case of a 50 years old male patient, referred to our department for hepatic lesion study. He presents a medical history of arterial hypertension and renal cysts and lithiasis. He had sporadic alcohol consumption and no history of drug consumption.
On a routine abdominal CT scan to evaluate renal cysts and lithiasis, was found in a normal liver, a 27 mm nodule in segment IV, hypervascular with practically continuous globular peripheral uptake and hypodense centre, that does not follow the density of the vascular structures (it is slightly less hypodense in the portal phase) and has some lavage and only slightly hypodense in the late phase, with the diagnostic conclusion of the most likely hypothesis as focal nodular hyperplasia (FNH) or adenoma.
We performed an abdominal ultrasound (US) and contrast enhanced ultrasound (CEUS) that showed a liver with normal echogenicity and structure, preserved dimensions and regular surface, and in the left hepatic lobe, segment IVb, iso to slightly hyperechogenic nodule with anecogenic central areas, with 24mm larger diameter (Fig. 1), without vascular doppler behaviour. (Fig. 2)

Figure 1. B-mode US.

Figure 2. CEUS.
After US contrast agent (Sonovue) injection the nodule presented a centripetal, globular and complete arterial hyperenhancement in the arterial phase (Video), with lighter hyper-enhancement in the portal phase (Fig. 3), and remaining isoenhanced with the parenchyma in the late phase (Fig. 4).
VIDEO . CEUS – arterial phase.
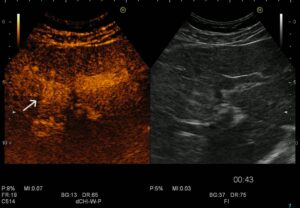
Figure 3. CEUS – portal phase.
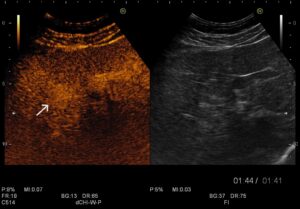
Figure 4. CEUS – late phase.
What is the most likely diagnosis?
Discussion
Hepatic hemangiomas are the most common benign liver lesions, with a prevalence of up to 20% in the general population. Although they are more frequently observed in women (4:1 ratio), they can also occur in men.[2] Histologically, hemangiomas consist of blood-filled vascular spaces separated by thin fibrous septa. While most are asymptomatic, larger lesions (>5 cm) may cause mass effect symptoms or complications such as thrombosis or rupture. Once diagnosed, no further follow-up is typically required.[3]
On B-mode US, hemangiomas typically appear as well-defined, homogeneously hyperechoic lesions with posterior acoustic enhancement. However, atypical presentations, such as hypoechoic or heterogeneous echotextures due to thrombosis, fibrosis, or necrosis, can mimic malignant tumors. Color doppler imaging generally shows minimal or absent vascularity.[4]
CEUS has proven to be a highly valuable imaging modality for the characterization of focal liver lesions (FLLs). It is particularly useful for evaluating indeterminate lesions identified on CT or MRI, thereby guiding clinical management and reducing unnecessary biopsies.[1]
The hallmark CEUS feature of hemangiomas is peripheral nodular enhancement in the arterial phase, with progressive centripetal fill-in and sustained contrast retention in the late phase. This pattern is highly specific and distinguishes hemangiomas from malignant lesions, which usually exhibit early washout. [4]
The alternative diagnoses were excluded. FNH typically demonstrates rapid arterial enhancement with a central scar and lacks the centripetal fill-in pattern characteristic of hemangiomas. Hepatic adenomas usually present with homogeneous arterial phase enhancement, rapid centripetal filling without nodular characteristics, and isoenhancement in the portal and late phases, which were not observed in this case. Given the absence of these alternative features, the imaging findings strongly support a diagnosis of hepatic hemangioma.
CEUS is a safe, non-invasiveness, and cost-effectiveness imaging technique for FLL characterization. It improves diagnostic confidence, minimizes patient anxiety, and reduces healthcare costs by limiting unnecessary follow-up imaging and invasive procedures. Based on the enhancement characteristics observed in this case, it is possible to make the diagnosis of hepatic hemangioma, a benign vascular lesion that typically does not require further intervention unless symptomatic.
References
- Dietrich, C.F., et al., Guidelines and Good Clinical Practice Recommendations for Contrast-Enhanced Ultrasound (CEUS) in the Liver-Update 2020 WFUMB in Cooperation with EFSUMB, AFSUMB, AIUM, and FLAUS. Ultrasound Med Biol, 2020. 46(10): p. 2579-2604.
- Caseiro-Alves, F., et al., Liver haemangioma: common and uncommon findings and how to improve the differential diagnosis. Eur Radiol, 2007. 17(6): p. 1544-54.
- Frenette, C., et al., ACG Clinical Guideline: Focal Liver Lesions. Official journal of the American College of Gastroenterology | ACG, 2024. 119(7): p. 1235-1271.
- Chaubal, N., et al., Contrast-Enhanced Ultrasound of Focal Liver Lesions. Seminars in Roentgenology, 2016. 51(4): p. 334-357.
Authors
Mariana Souto1,2,3, Sílvia Leite 1,2,3, Joana Magalhães1,2,3, José Cotter1,2,3
1 – Gastroenterology Department, Hospital da Senhora da Oliveira, Guimarães, Portugal;
2 – Life and Health Sciences Research Institute (ICVS), School of Medicine, University of Minho, Braga, Portugal;
3 – ICVS/3B’s – PT Government Associate Laboratory, Braga/Guimarães, Portugal


