US Quiz of the Month – janeiro 2025
Case Report
We present a 78-year-old male patient with a history of left radical nephrectomy for clear cell renal carcinoma, stage pT1bN0M0, in 2018, and a history of smoking (112 pack-years). He was referred to the Internal Medicine consultation in September 2024 for a non-productive cough of approximately 1-year duration. A chest CT was performed, revealing a nodular formation measuring 3.5 x 2.5 cm in the superior mediastinum, located posterior to the trachea and on the right side of the esophagus, as well as bilateral pulmonary micronodules/nodules, the largest measuring 13 mm. The patient subsequently underwent a PET-CT, which revealed a superior mediastinal lesion in the right paratracheal/esophageal region with increased glycolytic metabolism and pulmonary nodular formations with no increased FDG uptake.
AThe case was discussed in a multi-disciplinary team meeting and it was decided to perform endoscopic ultrasound (EUS) guided fine needle aspiration (FNA) for mediastinal nodule. In EUS showed a hypervascularized paraesophageal nodular lesion, with a maximum transverse diameter of 23.5 mm, that was punctured using a 22G needle (Fig.1).
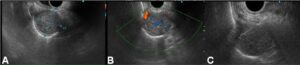
Figure 1. EUS: A,B – Hypervascularized paraesophageal nodular lesion. C – EUS-FNA.
What is the most likely diagnosis?
Discussion
Pathological examination showed clear cell renal carcinoma. In light of the recurrence of renal neoplasm, the patient began chemotherapy with pembrolizumab and lenvatinib.
Clear cell renal carcinoma is the most common renal neoplasm, with nephrectomy being the treatment of choice in early stages. The recurrence rate of T1bN0MO tumors after surgery is approximately 7% at 3 years, most commonly presenting as pulmonary metastasis, which may be associated with mediastinal lymphadenopathy. The assessment of mediastinal lesions presents a diagnostic challenge due to difficulties in accessibility for biopsy and the proximity to critical vascular structures. Endoscopic ultrasound-guided fine needle aspiration has been helpful in the diagnosis and staging of lesions near the esophagus, offering an alternative to more invasive procedures such as mediastinoscopy. We present this case for the technical challenge, highlighting endoscopic ultrasound as a diagnostic technique for paraesophageal mediastinal lesions. [1-3]
References
- Assisi D, Gallina FT, Forcella D, Tajè R, Melis E, Visca P, Pierconti F, Venti E, Facciolo F. Transesophageal Endoscopic Ultrasound Fine Needle Biopsy for the Diagnosis of Mediastinal Masses: A Retrospective Real-World Analysis. J Clin Med. 2022 Sep 17;11(18):5469. doi: 10.3390/jcm11185469. PMID: 36143116; PMCID: PMC9506435.
- Vilmann P, Clementsen PF, Colella S, Siemsen M, De Leyn P, Dumonceau JM, Herth FJ, Larghi A, Vazquez-Sequeiros E, Hassan C, Crombag L, Korevaar DA, Konge L, Annema JT. Combined endobronchial and esophageal endosonography for the diagnosis and staging of lung cancer: European Society of Gastrointestinal Endoscopy (ESGE) Guideline, in cooperation with the European Respiratory Society (ERS) and the European Society of Thoracic Surgeons (ESTS). Endoscopy. 2015 Jun;47(6):545-59. doi: 10.1055/s-0034-1392040. Epub 2015 Jun 1. Erratum in: Endoscopy. 2015 Jun;47(6):c1. doi: 10.1055/s-0034-1392453. Vasquez-Sequeiros, Enrique [corrected to Vazquez-Sequeiros, Enrique]. PMID: 26030890.
- Kim J, Ham WS, Park JS, Jang WS. Incidence and Pattern of Recurrence after Surgical Resection in Organ-Confined Renal Cell Carcinoma. Yonsei Med J. 2024 Nov;65(11):623-628. doi: 10.3349/ymj.2023.0587. PMID: 39439165; PMCID: PMC11519136.
Authors
Ana Rita Silva1, Nuno Nunes1, Nadine Amaral1, Francisca Côrte-Real1, Maria Pia Costa Santos1, Vítor Carneiro2, Maria Antónia Duarte1
1 – Serviço de Gastrenterologia do Hospital do Divino Espírito Santo de Ponta Delgada
2 – Serviço de Anatomia Patológica do Hospital do Divino Espírito Santo de Ponta Delgada


