US Quiz of the Month – March 2022
CASE REPORT
A 42-years-old Caucasian male, without relevant past medical history, was diagnosed with B-cell acute lymphoblastic leukemia. He completed the induction phase of the PETHEMA LAL Ph-2008 protocol, without complications. Later, the patient was readmitted to start the consolidation phase. However, it was noticed new-onset cytocholestasis and hyperbilirubinemia, without coagulopathy or encephalopathy. He had no personal or family history of liver disease. The metabolic, virological and autoimmune study was negative. Abdominal computed tomography scan revealed a liver with normal morphology and without hepatic metastasis or portal thrombosis. Magnetic resonance cholangiopancreatography showed normal intrahepatic and extrahepatic bile ducts. Endoscopic ultrasound (EUS) revealed no focal liver lesions. EUS-guided fine needle biopsy using a 22G needle was performed (2 passes; 22G Acquire, Boston Scientific) obtaining material that was sent for evaluation. The histological examination showed marked canalicular and hepatocytic cholestasis and ductopenia probably due to hepatic drug toxicity.
Ten days after the liver biopsy, the patient presented sudden epigastric pain. He was hemodynamically stable. The abdomen was soft, with epigastric tenderness, without rebound tenderness. Hemoglobin and hepatic profile remained stable and there was no elevation of inflammatory markers. The abdominal ultrasound (US) revealed a heterogeneous lesion with 56 mm located in segment VIII of the liver (Fig. 1).

Figure 1. Abdominal US: heterogeneous lesion with 56 mm located in segment VIII of the liver.
WHAT IS THE MOST LIKELY DIAGNOSIS?
DISCUSSION
The abdominal computed tomography scan revealed a hepatic pseudoaneurysm and an adjacent intrahepatic hematoma (Fig. 2).
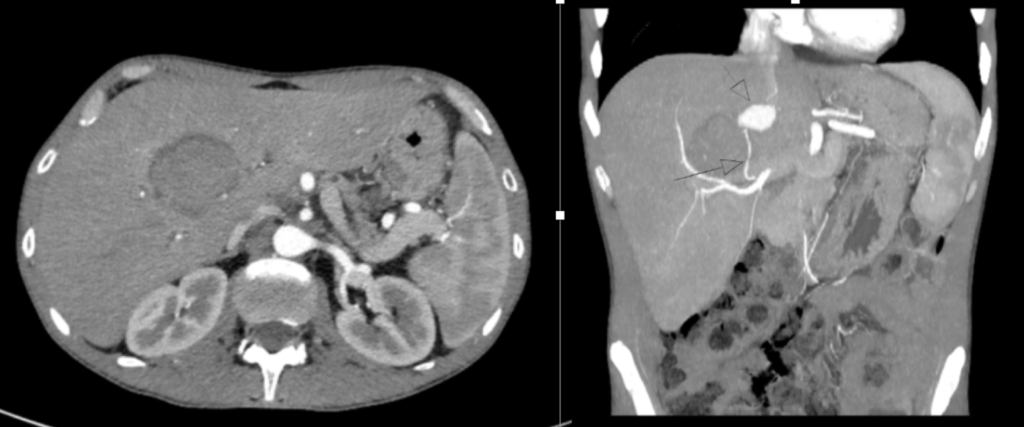
Figure 2. Abdominal CT (axial and coronal views): Hepatic pseudoaneurysm with 28 x 23 mm located in segment VIII with origin in a segmental branch of the main trunk of the right hepatic artery (arrows). It is located in the central topography, anterior to the intrahepatic segment of the inferior vena cava and cranial to the hepatic hilum. An adjacent intrahepatic hematoma with 54 x 45 mm was also identified (arrow).
After the diagnosis, the patient underwent a transcatheter arterial embolization. Complete embolization of pseudoaneurysm was accomplished after 3 embolization sessions, performed during 1 week. During hospitalization, the patient maintained hemodynamic stability, without the need for vasopressor support. The abdominal US showed a dimensional reduction of the pseudoaneurysm, with no evidence of active hemorrhage (Fig. 3). Currently, the patient is followed up in a Gastroenterology consultation and remains well after 5 months of liver biopsy.
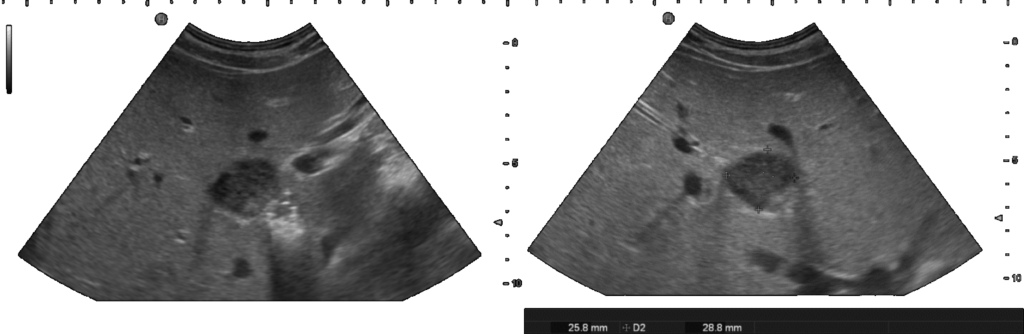
Figure 3. Abdominal US: Hepatic pseudoaneurysm located in segment VIII. It is identified echogenic material with associated shadow cone in relation to previous embolization.
A hepatic pseudoaneurysm is a false aneurysm that develops from leakage of an injured artery into the surrounding tissues forming a cavity outside the artery [1]. The development of a hepatic pseudoaneurysm is mainly described in patients after liver trauma but is also reported after invasive procedures such as percutaneous liver biopsies [2]. To our knowledge, hepatic pseudoaneurysm after EUS-guided liver biopsy has yet to be reported. However, pseudoaneurysm after EUS-guided fine needle biopsy from other organs, such as the pancreas, are described in the literature [3].
Symptoms of a hepatic pseudoaneurysm may vary from clinically silent to signs of rupture with intraperitoneal hemorrhage, rupture into the gastrointestinal tract, venous, portal or biliary system [1]. The diagnosis of a hepatic pseudoaneurysm is made with either arteriography, contrast-enhanced computer tomography or Doppler Ultrasound [1]. The most important differential diagnosis is a parenchymal hematoma. However, hepatic pseudoaneurysm can be distinguished from a hematoma as it continues to communicate with the artery [1].
All pseudoaneurysms require early treatment to prevent lethal adverse events. Angiography with transcatheter embolization is the initial treatment choice [4]. Several cases in the literature also describe the use of endoscopic ultrasound-guided coiling as a potential alternative to transcatheter embolization [5]. Surgery is indicated for hemodynamic instability, and uncontrolled hemorrhage after angiographic embolization [4].
REFERENCES
- Keeling AN, McGrath FP, Lee MJ: Interventional radiology in the diagnosis, management, and follow-up of pseudoaneurysms. Cardiovasc Intervent Radiol. 2009, 32 (1): 2-18. 10.1007/s00270-008-9440-3. Epub 2008/10/17
- Own A, Balzer JO, Vogl TJ. Bleeding hepatic pseudoaneurysm complicating percutaneous liver biopsy with interventional treatment options. Eur Radiol. 2005 Jan;15(1):183-5. doi: 10.1007/s00330-004-2287-3. Epub 2004 Mar 6. PMID: 15007619.
- Doo, Young-Jae, and Seung-Goun Hong. “Delayed Hemorrhage from Gastroduodenal Artery Pseudoaneurysm following Endoscopic Ultrasound-Guided Fine Needle Aspiration of Pancreatic Head Mass.” Korean Journal of Pancreas and Biliary Tract 23.4 (2018): 165-171.
- Reiter DA, Fischman AM, Shy BD. Hepatic artery pseudoaneurysm rupture: a case report and review of the literature. J Emerg Med. 2013 Jan;44(1):100-3. doi: 10.1016/j.jemermed.2011.08.021. Epub 2012 Jan 4. PMID: 22221986.
- Sharma, Malay et al. “EUS-guided coiling of hepatic artery pseudoaneurysm in 2 stages.” VideoGIE : an official video journal of the American Society for Gastrointestinal Endoscopy vol. 2,10 262-263. 19 Jul. 2017, doi:10.1016/j.vgie.2017.06.005
AUTHORS
Isabel Garrido1, Joel Ferreira Silva1, Rosa Coelho1, Susana Lopes1, Guilherme Macedo1.
- Gastroenterology Department, Centro Hospitalar Universitário de São João, Portugal


