US Quiz of the Month – Outubro 2024
Case Report
We present the case of a 64-year-old man with obesity, an active smoker with daily alcohol intake (60gr/day), presenting with epigastric abdominal pain associated with episodes of vomiting. Initial laboratory tests showed mild leukocytosis, elevated amylase and lipase, and normal liver function tests. He was hospitalized with the diagnosis of acute pancreatitis. Both lithiasis and metabolic etiology were ruled out. During the course of his illness, he developed systemic inflammatory response and respiratory dysfunction, requiring low-dose supplemental oxygen. A contrast-enhanced abdominal CT scan revealed inflammatory changes in the pancreas and peripancreatic tissues (Figure 1A) with an hypoenhancement area with 37×28 mm in the head of the pancreas (Figure 1B), suggestive of necrosis; intercurrent infection was ruled out.
After 9 days, he was discharged without the need for supplemental oxygen and with controlled abdominal pain.
As part of the etiological study of acute pancreatitis, an MRI of the abdomen was conducted 8 weeks after the initial hospitalization, revealing a 70 mm collection in the body of the pancreas suggestive of pancreatic necrosis, two peripancreatic pseudocysts each measuring 50 mm, and small cysts in the head of the pancreas. He was referred to our department for endoscopic ultrasound (EUS). The EUS revealed changes consistent with chronic pancreatitis, a main pancreatic duct of normal diameter, and two peripancreatic collections, the largest measuring 80×70 mm (Figure 2A), consistent with a pancreatic pseudocyst. A fine needle aspiration (FNA) was performed, and this etiology was confirmed by cytological and biochemical studies. The small cysts in the head of pancreas described in the MRI, revealed to be a multiloculated cystic lesion measuring 32×25 mm (Figure 2B). This lesion was also punctured and a mucoid content with positive string test was aspirated. Cytology showed mucinous cells with low grade atypia, and biochemical analysis revealed glucose <10 mg/dL and CEA 168 ng/mL, consistent with a mucinous lesion.
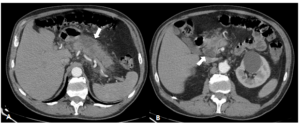
Figure 1. Contrast-enhanced CT of the abdomen. A. Diffuse pancreatic edema and stranding of the peripancreatic fat. B. Hypoenhancement area in the head of the pancreas.
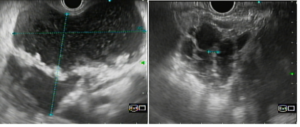
Figure 2. Endoscopic ultrasound. A. Anechoic lesion of 80 mm, thin wall, and echogenic material inside. B. Multiloculated anechoic lesion of 32 mm, with no hyperechoic areas within.
In our patient:
Discussion
This case involves a patient with multiple risk factors for acute pancreatitis. Although gallstone disease and alcohol are the two main causes of acute pancreatitis (1), it is essential to consider other causes that may have significant clinical implications for the diagnostic and therapeutic approach to patients, as they may necessitate interventions aimed at ruling out associated malignancy.
Pancreatic pseudocysts are encapsulated fluid collections with well-defined walls, usually extra-pancreatic, and often present as single or multiple unilocular cysts (2). IPMN are the most common type of pancreatic mucinous cystic lesions, with peak incidence occurring in the sixth and seventh decades of life. They can be either simple or multilocular, as in the case of this patient, and carry a risk of malignant transformation ranging from 1-38% (2).
In a patient with a history of acute pancreatitis, pancreatic cysts detected in CT/MRI are usually interpretated, by default, as pseudocysts. However, in our patient, the endosonographic characteristics of the pancreatic head lesion differ from the usual aspect of pseudocysts, so FNA was performed and cytological study confirmed a mucinous lesion, most probably a side brunch intraductal papillary mucinous neoplasm (SB-IPMN), harboring potential malignant risk.
Moreover, a “true” pancreatic cyst identified in a patient with history of pancreatitis should raise suspicion, as it could be the cause rather than the consequence of pancreatitis, and thus should not automatically be considered a pseudocyst (2). In this case, the cyst size of >3 cm and the episode of acute pancreatitis are considered worrisome features predictive of advanced neoplasia (high-grade dysplasia or cancer) (3), warranting further investigation.
Our goal in presenting this case is to remind that not every cyst in the context of acute or chronic pancreatitis is a pseudocyst. It is crucial to interpret these lesions cautiously, considering clinical and imaging characteristics that guide clinical decisions.
References
- Maderos M, Reber HA, Girgis MD. Acute Pancreatitis, a Review. JAMA. 2021;325(4):382-390
- Gonda TA, Cahen DL, Farrell JJ. Pancreatic Cysts. N Engl J Med. 2024 Sep 5;391(9):832-843
- Ohtsuka T, Fernandez-Del Castillo C, Furukawa T, Hijioka S, Jang JY, Lennon AM, Miyasaka Y, Ohno E, Salvia R, Wolfgang CL, Wood LD. International evidence-based Kyoto guidelines for the management of intraductal papillary mucinous neoplasm of the pancreas. Pancreatology. 2024 Mar;24(2):255-270.
Authors
Janeth Bejarano1 Pedro Moutinho Ribeiro1,2; Rosa Coelho1,2; Guilherme Macedo1,2
1 – Gastroenterology Department, Centro Hospitalar Universitário São João, Porto, Portugal
2 – Faculty of Medicine of the University of Porto, Porto, Portugal


